With increasing frequency Bodyscan customers will say the reason they have come for a DEXA scan is because they have read Outlive by Dr Peter Attia.
Peter Attia is an American-Canadian doctor, author and podcaster whose medical practice specialises in proactively lengthening its patients’ lifespan and simultaneously improving their ‘healthspan’ (ie, being healthy in older age).
Attia’s book, Outlive: The Science and Art of Longevity, has become an instant bestseller and reached number 3 in the Amazon charts within a month of publication.
In Outlive Attia says, “I insist my patients undergo a DEXA scan annually”. In this podcast Attia goes further and says, “We are really adamant that our patients get DEXA scans at least once a year. I think this is a very important thing to be doing.”
DISCOVER DEXA SCANS HEREBut why? How do DEXA scans assist, according to Attia, the pursuit of longevity and a better healthspan?
It’s because the DEXA scan report provides three metrics (provided by four data points) that are important indicators of overall physiological health. Significantly, the one metric “that most people care about when they get a DEXA scan” is, for Attia, the “least interesting”. This is body fat percentage, simply total fat mass divided by total body weight.
At Bodyscan we can definitely affirm Attia’s claims that body fat percentage is the main driver for customers wanting a scan and that DEXA scans are “very accurate at measuring fat.”
So, if not total body fat or body fat percentage, what are the three DEXA scan metrics that Peter Attia homes in on to start improving longevity?
They are:
- Visceral fat
- Bone mineral density
- Muscle mass
Peter Attia’s most important DEXA metrics:
1. Visceral Fat
Visceral fat is known as ‘bad fat’ and surrounds the internal organs within the abdominal cavity. In Outlive, Attia likens ‘normal’ subcutaneous fat (that’s fat stored beneath the skin) to water flowing into a bathtub from a tap. What we call ‘fat burning’, caused by a calorie imbalance, is analogous to the water emptying through the plug hole. The amount of fat (water level) will rise and fall depending on how many calories you consume (flow from the tap) and your energy expenditure (how quickly it drains away).
Attia says we each have our own genetic capacity to store fat – some people have a bathtub, others a full-size jacuzzi, others a small bucket. Irrespective of capacity, when the vessel fills up, the water (fat) spills over and ends up flooding places injurious to health. This is visceral fat.
In Outlive, Attia says, “It doesn’t take much visceral fat to cause problems.” Even a 40-year-old man with average (50th percentile) total body fat “would be considered at exceptionally high risk for cardiovascular disease and type 2 diabetes, in the top 5 percent of risk for your age and sex.” And it is then that Attia concludes: “This is why I insist my patients undergo a DEXA scan annually – and I am far more interested in their visceral fat than their total body fat.”

From Bodyscan’s vast database of UK DEXA scans and our experience in delivering them, we can add that visceral fat appears to ‘take off’ in our late forties and early fifties, most likely due to a slowdown in physical activity.
Different ethnicities carry different levels of visceral fat. Black people carry less visceral fat than white people who, in turn, carry less than South Asians.
Women have less visceral fat on average than men but, after menopause, the rate of increase in visceral fat matches or exceeds that of men.
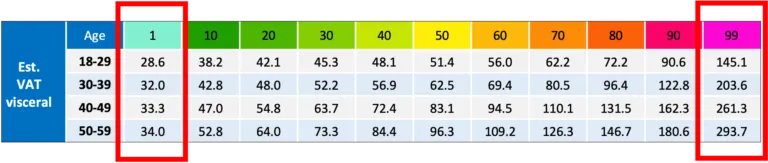
Measured by DEXA scan, medical thresholds have been applied to the VAT (visceral adipose tissue) result: below 100 is considered ‘normal’; between 100-160 (as in the example below) puts you at ‘increased risk’ of obesity-related diseases; and above 160 is categorised as being at ‘high risk’ of disease. The thresholds are non-discriminatory, which is why Bodyscan applies its expertise and experience in assessing you against a similar demographic (age, sex, ethnicity).
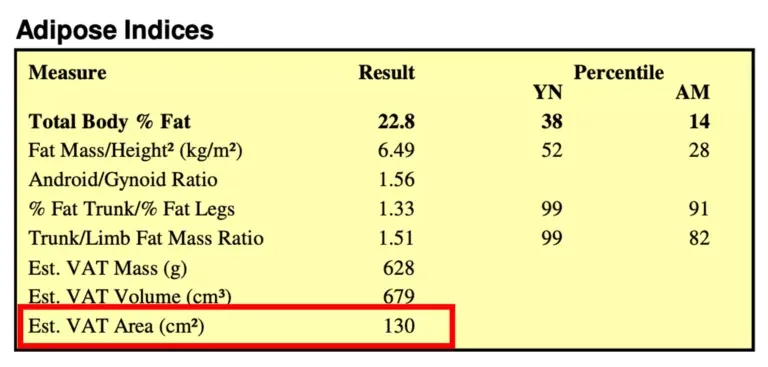
What’s also interesting (as you can see from the table below) is that, across the age groups from 18 to 59 (and above), at the low end visceral fat can remain very low, with no discernible change in the result. In contrast, the highest percentiles see visceral fat climbing higher and higher – for male over-50s it’s double (almost 300) the value for the under-30s (145). In the highest percentile, women’s visceral fat results are slightly higher (170 and 313 respectively).
 BOOK YOUR DEXA SCAN HERE
BOOK YOUR DEXA SCAN HERE
2. Bone Mineral Density
Outlive states a startling and confronting statistic: “the mortality from a hip or femur fracture is staggering once you hit about the age of sixty-five. It varies by study, but ranges from 15 to 36 percent in one year – meaning that up to one-third of people over sixty-five who fracture their hip are dead within a year.”
Bone fractures are more likely if bone density is low. Attia laments “classic Medicine 2.0”, whereby bone mineral density (BMD) is not routinely checked until women reach 65 and men 70 by which time “someone may be staring danger in the eye.”
In contrast, the Outlive author measures “BMD in every patient, every year, looking at both of their hips and their lumbar spine using DEXA. This also measures body fat and lean mass, so it’s a useful tool across all of the body-composition domains that we care about.”
It’s important, though, to draw a distinction between bone scans and body scans. Attia does not do that as clearly as he might in Outlive. Bone DEXA scans and body DEXA scans are two very different modalities. A body scan provides an indication of bone density, but a bone scan provides no information at all about body composition.
Even moreso than with visceral fat, which lies unseen in the abdomen, bone density cannot be known without the all-seeing eye of DEXA’s low-dose X-rays.
Low bone density (which increases the risk of fractures) is assigned a Z-score and T-score. These are medically significant mathematical rankings that compare your BMD with those of people the same age (Z-score) and those at the age of peak bone density (T-score). Low scores indicate osteoporosis or its precursor osteopenia. If you’re under 50, you want a Z-score above -2.0. If you’re over 50 a T-score above -1.0.
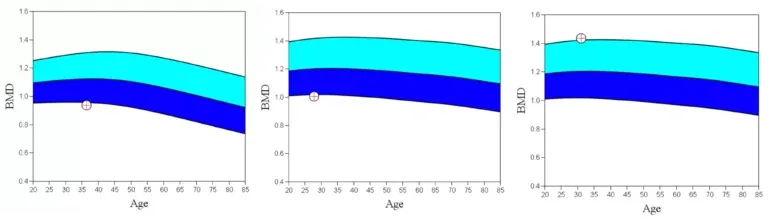
Whilst “Medicine 2.0” expects low bone density to affect only older people, certainly Bodyscan has encountered customers as young as in their 20s and 30s whose body-scan-BMD result has indicated osteopenia and osteoporosis – see charts above.
In Outlive, Attia has a four-point strategy to increase BMD, the second of which is “Heavy load-bearing activity. Strength training, especially with heavy weights, stimulates the growth of bone – more than impact sports such as running (though running is better than swimming/cycling).” Certainly, Bodyscan customers who do regular resistance training typically have higher bone density than those who don’t.
We go into the details of bone density results delivered by a DEXA body scan in this deep-dive video.
3. Muscle Mass
Attia is emphatic in Outlive about the need to preserve our muscle mass: “Continued muscle loss and inactivity literally puts our lives at risk. Seniors with the least muscle mass (also known as lean mass) are at the greatest risk of dying from all causes.”
Once more, he quotes a staggering statistic, this time from a Chilean study of 1400 people with an average age of 74. Of those in the lowest quartile for muscle mass, after 12 years about half of them were dead, compared to just 20 percent of those in the highest quartile.
Attia uses two datapoints from the DEXA scan to “triangulate” overall muscle mass for people of the same sex, age and ethnicity, normalised by accounting for their height.
These two datapoints are Lean Mass Index (LMI), and Appendicular Lean Mass Index (ALMI).
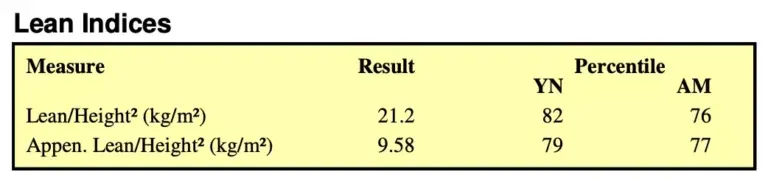
LMI is your total lean body mass (mainly muscle and organs) divided by your height-squared. ALMI is the same (lean mass in relation to height) but for your arms and legs only.
Because lean body mass is all fat-free soft tissue, your ALMI (lean mass in your limbs, adjusted for height) is essentially just muscle and removes any skewing associated with your organs in the trunk region. Without the organs, Attia refers to ALMI as a more “pure” measurement of muscle mass.
In this interview with Chris Williamson (clip below), Attia says, “Most people don’t know their ALMI. They don’t actually know how much muscle mass they have. They don’t know where they stack up for other people their age and sex and yet that’s also a highly, highly predictive metric of how long you’re going to live.”
Along with the medical thresholds of 100 and 160 for visceral fat, and Z- and T-scores for bone density, there are medical boundaries for ALMI too: sarcopenia (muscle wastage) is defined as a DEXA-assessed ALMI of below 7.23 for a man and below 5.67 for a woman when combined with a swift decrease in strength (eg, hand grip).
Interestingly, Peter Attia wants his patients to be “north of the 75th percentile” for FMI and ALMI – that is, more muscle for their height than 75% of people their age, sex and ethnicity. In Bodyscan’s experience, an amateur bodybuilder would be around the 80th percentile, so one might say that the emphasis the Outlive author places on muscle mass is ‘ambitious’ to say the least!
Follow Peter Attia’s Outlive advice and get your own DEXA scan
For all his chosen metrics, Attia assigns great importance to where a patient sits in relation to their peers; in other words their percentile rankings.
With more than 18,000 DEXA scans, Bodyscan has more comparison data and more qualitative experience than anyone to interpret your results as they relate to you and your goals. Your results will be plotted against those thousands of scans to give context to the numbers.
BOOK YOUR DEXA SCAN NOWAnd we’ll tell you what you have to do to reach a healthier percentile. To book your first DEXA body scan, click here.
Philip Chant
BodyScan Director